Travel Tips
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Search
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
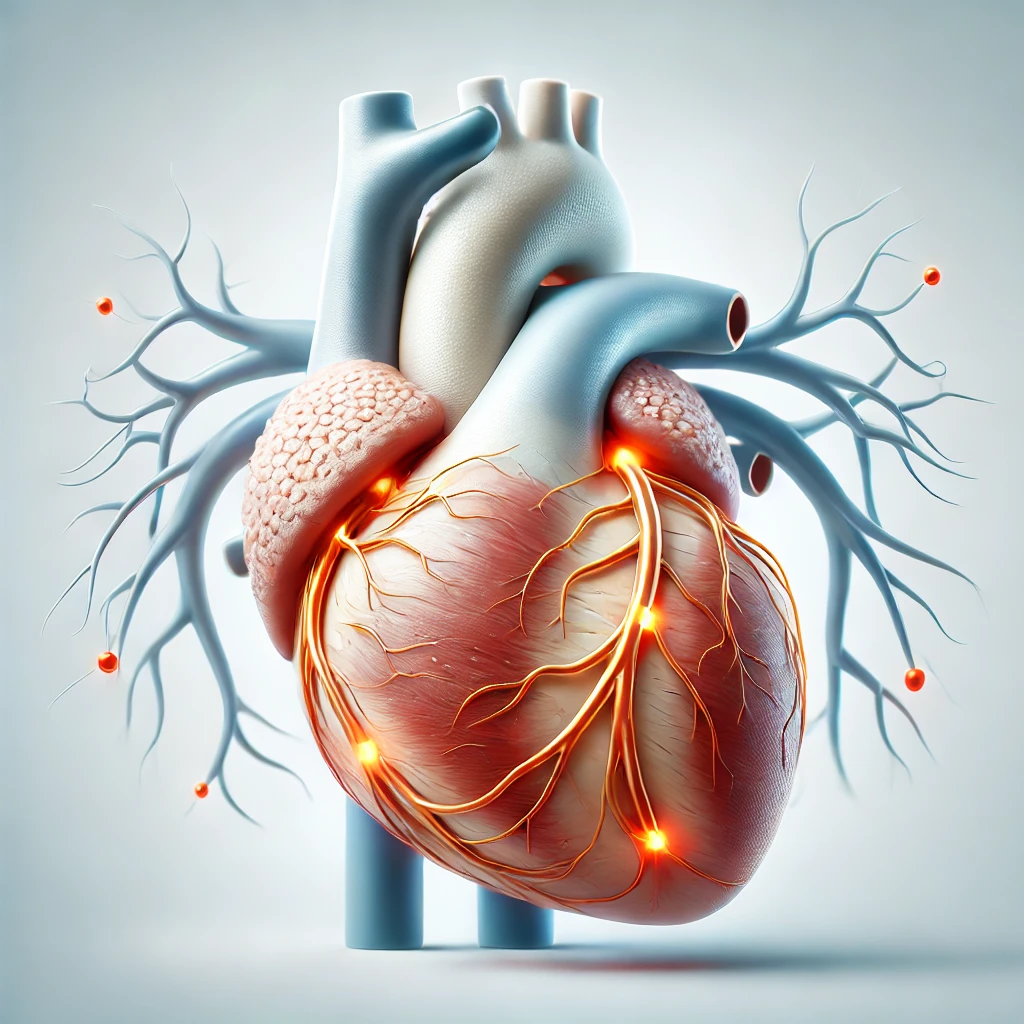
Atherosclerotic heart disease, also known as coronary artery disease, is a serious condition that affects the heart. It happens when fatty deposits, called plaque, build up in the coronary arteries. These plaques can harden and narrow the blood vessels, making it hard for oxygen-rich blood to reach the heart muscle.
It’s very important to understand atherosclerotic heart disease. It’s a top cause of heart attacks, strokes, and other heart problems. Knowing about it helps people take steps to prevent and manage it. This can improve their heart health.
Atherosclerotic heart disease, also known as coronary artery disease, is a condition. It happens when arterial plaque builds up in the coronary arteries. This narrowing and restricting of blood flow to the heart can harm its function.
The disease starts with fatty deposits, cholesterol, and other substances building up in the arteries. Over time, this arterial plaque hardens and grows. It narrowing the coronary arteries and blocks the flow of oxygenated blood to the heart muscle.
As the coronary artery narrowing gets worse, the heart gets less oxygen-rich blood. This can cause chest pain, or angina. It can also lead to other symptoms when the heart doesn’t get enough blood and oxygen.
Atherosclerosis can take different forms. There’s stable atherosclerosis, where plaque builds up slowly. And there’s unstable atherosclerosis, where plaque can rupture easily. This can cause blood clots and potentially lead to a heart attack.
“Atherosclerosis is a slow, complex disease process that can begin as early as childhood and progress over decades.”
Atherosclerotic heart disease is a major cause of heart problems. It’s influenced by several risk factors. Knowing these factors helps in preventing and managing the disease. Key contributors include high blood pressure, diabetes, smoking, obesity, and family history.
High blood pressure can harm the arteries’ inner lining, leading to plaque buildup. Diabetes, if not controlled, speeds up the atherosclerosis process. It does this by increasing inflammation and oxidative stress in the blood vessels.
Smoking is a known risk factor. The harmful chemicals in tobacco smoke damage the arteries’ lining, helping form plaques. Obesity, especially around the belly, raises the risk of atherosclerosis. This is because it’s linked to metabolic issues and inflammation.
Lastly, a family history of heart disease increases your risk of atherosclerosis. This shows the importance of genetics in the condition’s development. These risk factors can work together, making it essential to tackle them early for better heart health.
“Identifying and managing these risk factors is a crucial step in preventing and managing atherosclerotic heart disease.”
It’s important to know the early signs of atherosclerotic heart disease. These signs can range from mild discomforts to serious emergencies. Understanding these indicators helps people get medical help quickly and avoid serious problems.
Some symptoms need immediate medical help. They might signal a heart attack or other serious heart issue. These include:
Some people with atherosclerotic heart disease don’t feel any symptoms. This is called “silent ischemia.” It’s dangerous because it can make people wait too long to get medical help. Diabetes, older age, and some medicines can make silent ischemia more likely.
Knowing all the symptoms, from small to big, is key to catching atherosclerotic heart disease early. By being aware of these signs, people can protect their heart health. They can also get medical help fast when needed.
Atherosclerotic heart disease can sometimes develop without the classic symptom of angina pectoris. This is known as asymptomatic coronary artery disease or silent ischemia. People with this condition may have subclinical atherosclerosis without feeling the typical chest pain or discomfort.
Diagnosing asymptomatic coronary artery disease is challenging because there are no obvious symptoms. Regular check-ups and screening tests, like stress tests or imaging scans, are key. They help find this condition early, when treatments work best.
“Atherosclerotic heart disease without angina pectoris requires a high index of suspicion and vigilant screening to ensure timely detection and intervention.”
Understanding atherosclerotic heart disease without typical symptoms is crucial. Healthcare providers can then improve early detection and management. This helps improve the cardiovascular health of their patients.
Doctors use many ways to find and check atherosclerotic heart disease. They use tests to see how bad it is and how far it has spread. This helps them make a good plan to treat it.
Non-invasive tests are key in the first steps of checking for atherosclerotic heart disease. The ECG (electrocardiogram) checks the heart’s electrical activity. The stress test sees how the heart does under stress. Also, cardiac CT scans show detailed pictures of the heart and blood vessels, spotting plaque.
At times, doctors need to do more detailed tests. Coronary angiography is one. It uses a thin tube to see the heart’s arteries and find any problems.
Doctors also do blood tests to check the heart’s health. A lipid profile checks cholesterol and fats in the blood. This helps understand the risk of atherosclerotic heart disease.
| Diagnostic Test | Purpose |
|---|---|
| ECG (Electrocardiogram) | Measures the electrical activity of the heart |
| Stress Test | Assesses how the heart responds to physical exertion |
| Cardiac CT Scan | Provides detailed images of the heart and blood vessels |
| Coronary Angiography | Visualizes the coronary arteries and identifies blockages or narrowing |
| Lipid Profile | Measures cholesterol and other fats in the blood |
Doctors use different tests to understand atherosclerotic heart disease well. This lets them make a treatment plan that fits each person’s needs.
Atherosclerotic heart disease is a condition where plaque builds up in arteries. It needs a full treatment plan. This includes medicines, lifestyle changes, and medical procedures to manage it well.
Medicines are key in treating atherosclerotic heart disease. Statins help lower cholesterol and slow plaque growth. Antiplatelet therapy, like aspirin, stops blood clots and lowers heart attack risk. Beta-blockers control blood pressure and heart rate, easing symptoms and improving heart health.
Lifestyle changes are also vital. Eating a heart-healthy diet, exercising regularly, and managing stress help a lot. These actions can manage and prevent this condition.
| Treatment Option | Description |
|---|---|
| Statins | Medication that helps lower cholesterol levels and slow plaque buildup |
| Antiplatelet Therapy | Medication that prevents blood clots and reduces the risk of heart attacks |
| Beta-Blockers | Medication that controls blood pressure and heart rate |
| Lifestyle Changes | Adopting a heart-healthy diet, regular exercise, and stress management |
Combining medicines and lifestyle changes helps manage atherosclerotic heart disease. Regular check-ups and working closely with doctors are crucial. This way, a treatment plan can be made that fits the person’s needs best.
Living a heart-healthy lifestyle is key to preventing and managing atherosclerotic heart disease. Making smart food choices, staying active, and managing stress are important steps. These actions help protect your heart health.
Eating a heart-healthy diet is vital for your heart. Focus on whole foods like fruits, veggies, whole grains, lean proteins, and healthy fats. Cut down on saturated and trans fats, added sugars, and sodium. Eating more plant-based foods and seafood rich in omega-3s also benefits your heart.
Regular exercise keeps your heart healthy. Aim for 150 minutes of moderate or 75 minutes of vigorous aerobic exercise weekly. Activities like brisk walking, swimming, or cycling are great. Also, do strength training two to three times a week to build muscle and boost fitness.
Too much stress is bad for your heart. Try meditation, deep breathing, yoga, or hobbies that make you happy. Lowering stress can help your blood pressure, reduce inflammation, and improve your overall health.
“Incorporating lifestyle changes can have a significant impact on reducing the risk and managing the progression of atherosclerotic heart disease.”
By choosing a heart-healthy diet, staying active, and managing stress, you can prevent and manage atherosclerotic heart disease. These lifestyle changes can greatly improve your heart health and quality of life.
Treating atherosclerotic heart disease often involves a mix of medications. These drugs target different parts of the condition. They are key in managing the disease and lowering the risk of serious problems.
Statins are the main type of cholesterol-lowering drug used. They stop the liver from making too much cholesterol. This lowers LDL (bad) cholesterol levels. Statins help slow plaque buildup and reduce heart attack and stroke risks.
High blood pressure is a big risk factor for atherosclerosis. Medications like ACE inhibitors, ARBs, and calcium channel blockers are used. They help lower blood pressure and improve blood flow.
Anticoagulant and antiplatelet medications, such as aspirin, are often given. They prevent blood clots and reduce heart attack and stroke risks. These drugs help keep blood flowing smoothly.
| Medication Class | Mechanism of Action | Benefits | Potential Side Effects |
|---|---|---|---|
| Cholesterol-Lowering Drugs (Statins) | Inhibit cholesterol production in the liver | Reduce LDL (bad) cholesterol levels, slow plaque progression | Muscle pain, liver enzyme elevation, increased risk of diabetes |
| Blood Pressure Medications (ACE Inhibitors, ARBs, Calcium Channel Blockers) | Regulate blood pressure by various mechanisms | Lower blood pressure, improve blood flow | Dizziness, headaches, swelling, kidney function changes |
| Anticoagulants and Antiplatelets (Aspirin, Anticoagulants) | Interfere with blood clotting mechanisms | Prevent blood clot formation, reduce risk of heart attacks and strokes | Increased bleeding risk, gastrointestinal ulcers |
It’s vital to take medications as directed and follow up with your doctor. Working closely with your healthcare team is crucial. They can help find the best medication plan and watch for side effects.
“Medications play a vital role in the treatment of atherosclerotic heart disease, helping to manage risk factors, prevent complications, and improve overall cardiovascular health.”
For severe heart disease, doctors might suggest surgery or interventional treatments. These methods aim to improve blood flow and heart function. Angioplasty with stenting and coronary artery bypass grafting (CABG) are common options.
Percutaneous coronary intervention (PCI), or angioplasty, is a minimally invasive method. It uses a balloon-tipped catheter to widen narrowed or blocked arteries. A small mesh tube called a stent is often placed to keep the artery open.
Angioplasty and stenting are best for patients with single or limited blockages. These procedures can help relieve symptoms and lower the risk of heart attack.
Coronary artery bypass grafting (CABG) is a more extensive surgery for severe coronary artery disease. The surgeon creates a new path for blood flow around the blocked area. This is done using a blood vessel from another part of the body, like the leg or chest wall.
CABG is recommended for patients with multiple or complex blockages. It can greatly improve blood flow and lower heart attack risk. However, it carries a higher risk of complications than less invasive methods.
The choice between PCI and CABG depends on several factors. These include the blockage’s severity and location, the patient’s health, and their preferences. Doctors and patients work together to find the best treatment.
Living with atherosclerotic heart disease can be tough, but it’s possible to live a healthy life. Understanding cardiac rehabilitation, building a support network, and using management strategies are key.
Cardiac rehabilitation programs help manage heart disease. They include:
Joining a cardiac rehab program can greatly improve your health and happiness. It helps you manage your heart disease better.
Having a strong support network is crucial. It includes:
A supportive network makes dealing with heart disease easier. It shows you’re not alone.
Managing heart disease long-term needs a plan. It includes:
By following these steps, you can reduce risks and improve your life with heart disease.
Managing atherosclerotic heart disease needs a team effort. With the right support, knowledge, and strategies, you can live well despite the challenges.
Atherosclerotic heart disease is a serious health issue. It needs careful prevention, early detection, and full management. Knowing how plaque forms, identifying risk factors, and watching for symptoms helps keep your heart healthy.
Preventing this disease starts with lifestyle changes. Eating well, exercising regularly, and managing stress are key. Also, new research in heart disease prevention and care is promising. It could help fight this condition even more.
We must keep spreading the word, encourage early action, and support new treatments. Together, we can help people take care of their heart health. This way, we can make the future brighter, where heart disease is better understood and prevented.
Comments